Our
Plan
Our strategic plan helps us make choices that push us towards our newschool direction.
We are choosing team-based care and exploring ways to incorporate more interprofessionalism into primary care delivery.
We are choosing to address power dynamics and inequities by elevating the role of community in all aspects of the department’s work. This involves deeper and broader engagement with patients and families as well as more inclusion of learners and community partnerships.
We are choosing to embrace and foster the technologies that enhance the patient-provider experience and facilitate more equitable care delivery.
We are choosing to train learners and faculty who are not only clinical experts, but reflective and socially conscious so that they may deliver the best possible care for any person they encounter and sustain their own wellbeing throughout the most challenging days on the job.
We are choosing to build our own internal community by creating a network for our department to collaborate, coordinate and connect in order to learn from each other’s successes and challenges, find opportunities to work across sites and focus areas, and be part of the vibrant community within the DFCM.
Why-What-How
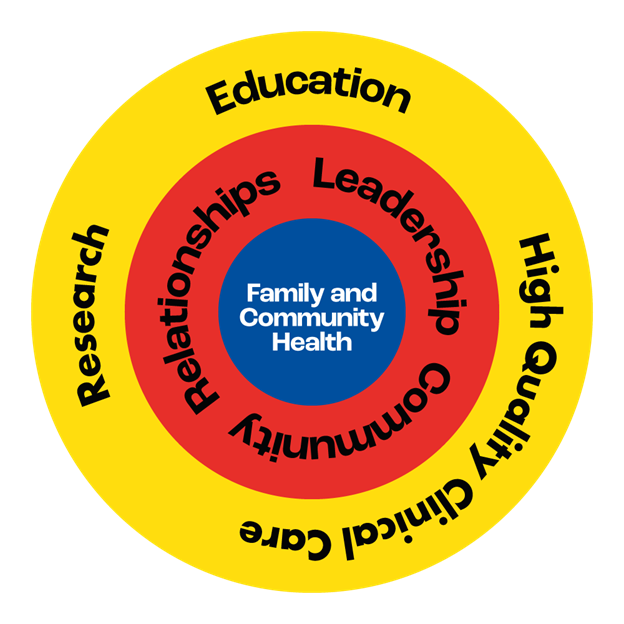
WHY: Ultimately, our aim in everything we do is to work towards family and community health.
WHAT: With this plan, we are adding three lenses with which we can assess and prioritize the actions we take, concentrate our energy, and focus our strategic intention: community, relationships, leadership.
HOW: The core tools of our work remain education, research, and high-quality clinical care.
Community
Community refers to the expansive network of people we serve and want to serve. This is about where people live their lives – bridging the gap between academic medicine and the experiences of the people who use, seek or need healthcare services. We don’t build bridges to community alone; we do so through partnerships with trusted organizations that have long histories of community-embedded work. Furthermore, we appreciate that each community has their own specific conditions and needs that must be considered and addressed in deep collaboration with those groups and with purpose-fit approaches.
Leadership
Leadership entails both achieving excellence and lifting everyone up collectively. Rather than a hierarchical approach, the work of leadership is about partnering to help shape the system, address inequities by providing resources and capacity, and excelling in those areas that matter most to the department and our people. The work of leadership brings our scholarly and academic skills to the task of improving health systems, locally and internationally.
Relationships
Relationships means focusing on connection and collaboration. We are committing to build and steward partnerships and synergies within and between the groups that the department touches: learners, staff, faculty, alumni, patients, families, partners, and beyond. We will work to develop and maintain connections that go beyond our silos, sites, and areas of focus and propel newschool possibilities for innovation, coordination, and partnership across our education, research and QI work.
“We need to treat cultural safety like any other kind of expertise and value it the same way”
Summary
COMMUNITY
– Invest in community partnerships across our Education, Research and Quality and Innovation work.
– Expand and enhance the community-based experience of learners.
– Optimize patient and community health outcomes by supporting, connecting and upskilling health care providers.
“It’s not about EDI which is very corporate – it’s about justice. When we have a better understanding of the pieces and practices within us that are unjust, we will be better able to serve our communities.””
RELATIONSHIPS
– Maximize our impact and visibility through deepened engagement across the Temerty Faculty of Medicine, Dalla Lana School of Public Health, the University of Toronto.
– Connect and support the DFCM community of learners, faculty, and alumni.
– Build and sustain more collaborative relationships with our patients and communities to guide our work.
– Amplify the voice and unlock the academic potential of community sites and faculty in the community in order to better represent the needs and perspectives of those they serve.
LEADERSHIP
– Elevate our position as a socially accountable, equity-focused academic leader for our faculty, learners, and staff.
– Lead and inform health system improvement, working collaboratively with local and global health system partners.
– Empower our faculty, staff and learners to prioritize personal leadership by embracing and adopting practices that promote their wellbeing and that of their colleagues in order to foster excellence in care, education, and scholarship.
– Support the self-determination of Indigenous health leaders and communities.
– Help scale health technologies and innovations that enhance patient-practitioner relationships.
Community
C1. Invest in community partnerships across our Education, Research and Quality and Innovation work.
C1.1 Create a Vice Chair Community and Partnerships role to develop, build, and steward impactful partnerships with community organizations and groups, Public Health Units, and other health system and social service organizations and associations (especially those serving equity-deserving communities), to promote better health outcomes.
C1.2 Improve access and attachment for communities most in need of care by collaborating with partner organizations. (This action will connect with the work of the OHSP, L2.1)
C1.3 Meaningfully involve every DFCM site in addressing the gaps in primary care access and attachment for First Nations, Inuit, and Métis communities, including by partnering with Indigenous health organizations and other agencies.
C1.4 Collaborate with our global and international partners to advance high-quality primary and emergency care around the world, leveraging DFCM expertise in education, research and QI.
C2. Expand and enhance the community-based experience of learners.
C2.1 Increase opportunities for medical learners to engage with community organizations and providers, through clinical and non-clinical community-based opportunities.
C2.2 Further embed learners in high-functioning teams and enhance opportunities for interprofessional healthcare team members to participate fully in the work of DFCM.
C2.3 Embrace a community-serving mindset in the curriculum that pays special attention to health equity in considering population health outcomes and social & structural determinants of health, including training in patient and system advocacy.
C.3 Optimize patient and community health outcomes by supporting, connecting and upskilling health care providers.
C.3.1 Build on our partnership with the OCFP to continue and develop the COVID-19 Community of Practice program and capacity building work for primary care providers in Ontario and beyond.
C.3.2 Build Continuing Professional Development and other programs to support primary care practitioners to integrate evidence into their practice and advance data-driven improvement for the benefit of their patients and communities.
C.3.3 Establish and convene a Black Health Advisory Table with the aim of advancing health in Black communities and advising the department on ways to support Black faculty and learners.
C.3.4 Build and steward strong internal partnerships across DFCM sites, divisions, professions, and wherever DFCM faculty practice to support our communities.
C.3.5 Leverage the expertise in our Divisions to provide meaningful upskilling for physicians practicing both comprehensive and enhanced skills family medicine.
Relationships
R.1 Maximize our impact and visibility through deepened engagement across the Temerty Faculty of Medicine, Dalla Lana School of Public Health, the University of Toronto.
R.1.1 Increase the presence and connection for DFCM across TFoM, DLSPH, and the U of T more widely to:
a) further integrate already developed systems and practices such as e-learning and EDI practices developed through Temerty ODI or U of T Scarborough;
b) increase presence across the spectrum of education;
c) enhance research collaborations and opportunities for clinician investigators, graduate students; and
d) strengthen existing interdepartmental partnerships within teaching sites and divisions and increase representation, leadership and role of family medicine across diverse practice settings.R.1.2 Support the OHSP's work in health system reform through a deeper connection with the U of T government relations office.
R.1.3 Develop a greater presence for DFCM in undergraduate programs and activities and TFoM admissions processes to encourage more uptake of generalism and more graduates practicing comprehensive care.
R.1.4 Explore the possibility of becoming the administrative home for TFoM and DLSPH's potential Planetary Health EDU
R.2 Connect and support the DFCM community of learners, faculty, and alumni.
R.2.1 Use DFCM Communications vehicles to share stories, build common purpose and celebrate our members across community sites, in the community, across our diverse teaching sites, divisions, professions and practices.
R.2.2 Create and implement the "DFCM Connects" network, using online platforms to share experiences, centralize knowledge, and communicate within and across all DFCM sites, divisions, practices, professions, and faculty locations.
R.2.3 Through the work of the OHSP and beyond, strengthen supports for graduates in their first five years of practice by offering extended mentorship, as well as additional CPD in order to provide early career guidance that meets a variety of needs.
R.2.4 Develop an alumni network and communications opportunities for alumni to collectively support each other and stay connected to DFCM.
R.3 Build and sustain more collaborative relationships with our patients and communities to guide our work.
R.3.1 Expand and strengthen the PFAC and other methods of patient and community engagement to build deeper opportunities for integration and co-design with patients and their families into DFCM research, education, and high-quality clinical care.
R.3.2 Support and collaborate with the Summer Mentorship Program and the communities it reaches in order to introduce family medicine to high school students and build interest and involvement with DFCM in students and their communities.
R.3.3 Work with people in communities facing systemic and structural inequities to amplify their most urgent health concerns and ensure these concerns are integrated in DFCM research, education, and the high-quality clinical care we deliver.
R4. Amplify the voice and unlock the academic potential of community sites and faculty in the community in order to better represent the needs and perspectives of those they serve.
R.4.1 Strengthen central DFCM supports for research at community sites and by community-based researchers with a goal of improving impact, building capacity and increasing research at community sites by 50% over 5 years.
R.4.2 Strengthen central DFCM supports for education and education scholarship at community sites and for faculty in the community, including across the divisions.
R.4.3 Ensure community sites, faculty in the community, and faculty across divisions and interprofessional streams are represented appropriately in Working Groups, DFCM Communications, allocation of resources, and staffing considerations.
Leadership
L.1 Elevate our position as a socially accountable, equity-focused academic leader for our faculty, learners, and staff.
L.1.1 Dedicate resources and supports to recruitment, retention, and promotion of learners, faculty and staff from equity-deserving communities and ensure that the environment they join is safe, supportive and respectful.
L.1.2 Establish a staff role focused on improving and expanding internal EDIIA practices starting with collecting and analyzing equity-based data and determining ambitious, quantitative goals.
L.1.3 Prioritize equitable health care, anti-racist, and anti-oppression approaches by offering mentorship, training and continued professional development for learners, staff and faculty tied to accountability.
L.1.4 Develop a Health Humanities Lead role to promote and embed creative and critical lenses across all curricula/learning activities, in order to help address hidden curricula, cultivate reflective practice among care providers, and develop more techniques and opportunities to support faculty, staff, and learner wellness.
L.1.5 Increase mentorship and education for all levels of learners focused on system navigation, practice management, and administration to appropriately prepare graduates to be able to work in comprehensive family medicine and community practice settings.
L.1.6 Become best in the world for research impact and scholarship capacity with associated metrics connected to grants, publications, altmetrics and narrative reports.
L.1.7 Demonstrate global leadership in virtual education and education about how to carry out virtual care, building on existing successes across the department.
L.1.8 Cultivate relationships with new global partners to enhance collaboration on high-quality scholarship related to primary care and increase dissemination through publications, conferences and events.
L.1.9 Prioritize the establishment of endowed chairs in Family Medicine Leadership (linked to the role of DFCM Chair); Education (linked to the role of Vice Chair education); and key scholarship priority areas at DFCM centrally and in partnership with each one of our 15 hospital sites.
L.1.10 Work closely with the Advancement team at TFoM to create an ambitious fundraising campaign to support all of the priorities and actions in this plan.
L.2 Lead and inform health system improvement, working collaboratively with local and global health system partners.
L.2.1 Develop and sustain the Office of Health System Partnership (OHSP) to focus on system priorities across the quintuple aim, such as those articulated by Ontario Health in 2022:
a) Covid recovery;
b) Attachment to primary care;
c) Health Human Resource Planning, and;
d) Primary Care Engagement.L.2.2 Re-focus UTOPIAN to advance the dual goals of "best in class care" in DFCM practices and "connected primary care research" through POPLAR and other key data holders in health and social care. Review and implement recommendations from the UTOPIAN external review to be completed October 2022.
L.2.3 Strengthen inter-professionalism and enable progress towards purposeful integrated and effective team-based care including exploring partnerships for developing new roles for unregulated primary care workers such as scribes, community health workers, peer support workers and others to grow a fit-for-purpose primary care workforce.
L.2.4 Expand the Physician Assistant program to support growth, including advocating for the profession, supports for PA faculty, and promotion of practice integration of PAs in primary care practices, especially at sites with DFCM physician faculty practice.
L.2.5 Establish the role of Global Lead within the OHSP reporting directly to the chair to foster and oversee the development, integration and dissemination of primary healthcare-related innovations, and play a lead convening role to set an agenda with global thought leaders.
L.2.6 Under the leadership of the Global Lead, renew designation as a WHO Collaborating Centre and:
a) contribute to 10 WHO deliverables over the next five years;
b) involve at least one faculty and/or learner from every DFCM site and five faculty in the commuity in WHO-related work over the next 10 years;
c) include at least two colleagues from low and middle income countries in all WHO and/or international DFCM projects; and
d) deepen international education offerings in partnership with the OES and Education portfolios to strengthen primary care capacity globallyL.2.7 Harness departmental experience and provide thought leadership on the role that family medicine can play in responding to and preparing for future pandemics through growth of the Division of Clinical Public Health and a Clinical Public Health lead role in the OHSP.
L.2.8 Be a leading voice locally and globally in (the media, academia, and in the public sphere) in recognizing, shaping, highlighting, and advancing recognition of the value of family medicine as the foundation of a well-functioning healthcare system.
L.3 Empower our faculty, staff and learners to prioritize personal leadership by embracing and adopting practices that promote their wellbeing and that of their colleagues in order to foster excellence in care, education, and scholarship.
L.3.1 Shift criteria related to admissions and promotions to respect and recognize non-traditional value and impact from staff, learners, and faculty including relationship-building, mentorship, & community responsiveness and support.
L.3.2 Offer, resource, and incentivize wellness tools that are varied and variable in order to suit different needs such as peer support groups and opportunities for reflective, narrative and other arts-based practices.
L.3.3 Consider every opportunity, including resources for new or adjusted staff roles, to assist staff, faculty and learners in making more space for their top of scope work and wellbeing by:
a) developing tools and supports that promote efficiency;
b) removing or making optional elements of process, learning, or habit that are not essential; and
c) re-assigning tasks and actions to those best suited and equipped to manage them.
L.4 Support the self-determination of Indigenous health leaders and communities.
L.4.1 Nourish, provide for and protect the Indigenous Leadership Circle which will be adequately resourced and include a Council of Elders.
L.4.2 Make space and opportunity for Indigenous leadership at the highest levels in the department.
L.4.3 Implement mandatory cultural safety training at all levels within the department through the SAN’YAS anti-racism Indigenous Cultural Safety Training Program (or equivalent evidence-based programs) in order to actively respond to the calls to action of the TRC and other relevant reports.
L.4.4 Develop a physical space for connection and mentorship for Indigenous learners, staff and faculty within DFCM
L.5 Help scale health technologies and innovations that enhance patient-practitioner relationships.
L.5.1 Champion technologies, innovations and strategies for technology integration that reduce the administrative burden on practitioners and that enhance connection with patients. and between providers.
L.5.2 Building on the infrastructure of UTOPIAN/POPLAR, support emerging technologies and innovations that improve the quality of patient care and the ability to harness data to benefit research and practice.
L.5.3 Transition EXITE to a "DFCM Incubator" focused on technology-enabled education and education for technology-enabled collaborative team-based care.
“If I could choose to live in any time of history, I would choose tomorrow.”
To accomplish the goals we are setting for ourselves and implement each of the actions, the department requires the following four resources.
People: We will develop and support the people, roles, and capacities that we need to accomplish the actions we are committed to.
Money: We will work with the University of Toronto and Temerty Faculty offices of advancement to raise philanthropic funds to support our ambitions. We will continue to seek out all available appropriate funding that is relevant to our work.
Technology: We will update our systems and integrate new technologies to align with the needs of our teams and the aspirations of our work. We will work closely with our IT staff and our faculty working on and with technology to ensure we are pursuing the most efficient and effective hardware and software solutions for our collective needs.
Communication: We will work with our internal and external communications teams to build our networks and share our stories. We will reassess our communications vehicles and prioritize those that allow us the most effective outreach.
Definitions:
Community Sites: Community sites are not fully affiliated with TAHSN hospitals. These include:
Humber River Hospital
North York General Hospital
Oak Valley Health- Markham Stouffville Hospital
Royal Victoria Regional Health Centre, Barrie
Southlake Regional Health Centre, Newmarket
Scarborough Health Network
Toronto East Health Network- Michael Garron Hospital
Trillium Health Partners- Credit Valley Hospital
Unity Health Toronto- St. Joseph’s Health Centre
Faculty in the Community: Faculty in the community are practicing family doctors and other health care professionals who spend much of their clinical time in office-based or other non-hospital based settings.
Primary Health Care: Primary health care refers to an approach to health and a spectrum of services beyond the traditional health care system. It includes all services that play a part in health, such as income, housing, education, and the environment.
Primary Care: Primary care is the element within primary health care that focuses on health care services, including health promotion, illness and injury prevention, and the diagnosis and treatment of illness and injury.
Generalism: Offering comprehensive care.
Equity-Deserving Communities: These are the communities that have historically been disadvantaged by structural and systemic inequities and are often underserved and at risk of worse health outcomes.
Questions to Consider
We can ask ourselves a few key questions that will help us know if an opportunity or a project is aligned with our values, goals, and interests.
Does this deepen our commitment to, and collaboration with, community, to understand needs and inform our education, research and high-quality clinical care?
Does this build and strengthen our relationships within the DFCM, the University, the healthcare ecosystem, and more broadly?
Does this help demonstrate academic, systemic and/or personal leadership that prioritizes and embeds wellbeing; social accountability; health equity; and Equity, Diversity, Inclusion, Indigeneity, and Accessibility (EDIIA)?
Leadership Circles
Internal Leadership Circle:
Dana Arafeh, Ali Damji, Katrina Darcel, Risa Freeman, Ruth Heisey, Tara Kiran, Megan Landes, David Makary, Danielle Martin, Allyson Merbaum, Stu Murdoch, Donatus Mutasingwa, Elizabeth Niedra, Onye Nnorom, Amy Noise, Julia Pasquale, Katherine Rouleau, Peter Selby, Mruna Shah, Suzanne Shoush, Janet Smylie, David Tannenbaum, Caroline Turenko, Ross Upshur, David White, Quentin Wong, Catherine Yu
Indigenous Leadership Circle:
Sarah Park, Suzanne Shoush, Janet Smylie, Joel Voth
External Leadership Circle:
Beth Coleman, Monique Crichlow, Anna Greenberg, Martin Marshall, Notisha Massaquoi, Sarah Newbery, Robert Phillips, Jane Philpott, Jennifer Rayner, Jack Westfall, Ruth Wilson
Lived Experience Leadership Circle:
Amadou Barry, Maggie Brackley, Sharee Clark, Gerald Crowell, Sean Deschamps, Anu Dhir, Isabelle Duchaine, Tugba Karademir, Judy Katz, Katelyn Moore, Lisa Newman, Claire Wootten, Atif Zia
2022 Workshops
Social and Ecological Accountability - Monday, August 8
EDI - Monday, August 8
Image & Brand - Wednesday, August 10
High-Quality Clinical Care - Tuesday, August 16
Wellness, Arts and Humanities - Wednesday, August 17
Research - Monday, August 22
Department in the Community - Thursday, August 25
International Collaboration - Tuesday, August 30
Health System Partnerships - Wednesday, August 24
Generalism as Advanced Practice - Wednesday, September 7
Technology and Digital Tools - Thursday, September 8
Education - Thursday, September 8