Strategic
Context
Strategic plans serve a number of functions – to orient, to align, to connect, to focus, to propel.
In the third year of the pandemic, primary care providers, scholars and our patients are feeling at times exhausted and demoralized by COVID-19 and its many ripple effects. We can honour the experiences of our patients, colleagues and communities by learning from them – which is exactly what a university department is positioned to do. It falls to DFCM to draw lessons from this crisis, combatting burnout with shared purpose.
As the largest department of family and community medicine in the world, we have a duty to take on some of the biggest challenges facing the healthcare system, the wellbeing of our communities, and the training of future practitioners. DFCM must act as a leader in foregrounding the value of primary health care and the necessity of health equity.
And for this we need a new plan, new energy, and newschool thinking.
Over the past 52 years, the department has achieved incredible things, from the growth and expansion of our residency programs to the formation of our Divisions, the birth of UTOPIAN, the establishment of our Quality and Innovation work, the introduction of our WHO Collaborating Centre on Family Medicine and Primary Care and so much more. We have made it clear that DFCM at the University of Toronto has what it takes to lead the world in academic family medicine, not just because of our size, but because of our shared values, our passion for meaningful work and our care for one another. It is time for us to continue our tradition of excellence in family and community medicine education, research and high-quality clinical care with a renewed focus and ambition – to apply our tremendous skills to a newschool of thinking about the role of family medicine in the creation of healthy communities.
This plan sets out to guide us – to provide a map as we navigate the territory of our daily work.
Our leadership, faculty, staff, and learners now need to align our structures, attitudes, and approaches with our core values and our desire to see better health outcomes for the most underserved communities. The plan will also act as an invitation to our local, national and global partners, patients, and communities to engage with us. Together, we must be active collaborators if we are to achieve our ambitious goals. As colleagues and individuals, the plan reminds us to do all we can to support the health and wellbeing of our people – the most important resource we have.
“The map helps us to find our way, but knowing the territory from the map is not the same as knowing it by dwelling in it… If we are to be healers as well as technicians, we have at some point to set aside our maps and walk hand-in-hand with our patients through the territory.”
Much has changed since our last strategic plan.
The global pandemic has exhausted health system resources. Social movements for reconciliation with Indigenous communities, for racial justice and decolonization, and for institutional transformation in service of equity, diversity, inclusion and accessibility have changed the landscape in which we work and live. The demands to look upstream at the social determinants of health and health equity are growing as the evidence mounts that downstream thinking is inadequate to address the health challenges communities face. Family and community medicine must respond to these imperatives with a newschool of accountability and equity.
At the same time, the daily practice of teaching, learning, engaging in scholarship and clinical care is palpably different than it was three years ago. The things that clinicians love about practicing family medicine are often getting buried under less meaningful work, and that has an effect on recruitment and retention. There have been significant advances in virtual care, machine learning, and other technologies to advance high-quality patient-centred care, but some of these are inhibiting the human connection that lies at the core of our discipline. Our communities are aging and the complexity of the conditions family doctors and primary care teams manage is increasing – whether we work in office-based settings, emergency departments, patients’ homes, long-term care facilities, or on the streets of Canada’s largest city. We are concerned about the health of people but also of our planet, and must consider the ways that care delivery and healthcare infrastructure can evolve to respond to climate change and support planetary health with a newschool sustainability.
While the trajectory of COVID-19 and its long-term implications are unclear, we are certain that primary care must play a strong role in supporting public health and responding to the next phases of this pandemic and any future public health emergency. The trust that exists between patients and their primary care providers, and the longitudinal and relational nature of that care, is our most important tool. Relationships are the beginning, middle and end of our discipline and must therefore be at the core of any plan for the future.
Health systems built on a strong foundation of primary care and family medicine deliver better outcomes, more equitably, at lower cost. This evidence must be at the core of pandemic recovery locally, nationally, and internationally – and it falls to us to ensure that happens. Whether it’s about public perception, government policy, professional accountability, community responsiveness, or provider wellbeing, we have a newschool responsibility to solve the challenges we face. We owe it to our learners and our communities to bring the full force of our creativity, passion and skills to the table. In doing so, we can re-ignite our love for family and community medicine.
“Primary health care is where the battle for human health is won and lost.”
The energy of the faculty, staff and learners in this department is strong and steady, but when it wavers, we lift each other up. We know that the specialty of generalism focuses on relationship-based care, and it also requires elevated clinical expertise, making primary care incredibly rewarding. We need to share the stories, the data, and the heart of our discipline with the world with a newschool message.
This plan charts the path forward with
new vision, new priorities, and new ambition.
The strategic planning process was a conversation by design. Beginning two years into the pandemic, it was an opportunity to reconnect and try to make sense of what the last few years had been, while looking with hope towards the future.
We began by developing our What’s At Stake document to set the stage for our process, outline some of the major issues facing primary care, and undertake a brief environmental scan to see how other family and community medicine departments are approaching their work.
We established and convened our leadership circles. The Internal Leadership Circle included members of the department’s leadership as well as representatives from staff, all sites, and a variety of important perspectives. The External Leadership Circle was comprised of experts in the field from across the city, the province, and the United States to share insights and present an outside eye on the themes and priorities that were emerging from our process. Our Lived Experience Leadership Circle included a group of patients and community members from DFCM clinical sites who were able to bring the public’s voice into our process and help us see how family medicine is perceived and experienced by those receiving care. Together with these circles, we engaged with the Indigenous Leadership Circle, a group of DFCM faculty who identify as Indigenous and helped ensure that the priorities of Indigenous healthcare and leadership were approached appropriately and embedded in this plan.
In addition to the work of these leadership circles, we had many (many!) conversations. Staff, faculty and learners discussed their hopes for the plan in their committees and one-on-one, and we launched a department-wide survey that had over 250 responses. We uncovered the themes, priorities and ambitions being considered across the department. We also heard concerns about burnout and trepidation about adding on new work – reminding us that in order to achieve our ambitious goals, we will also need to have the courage to make space for it.
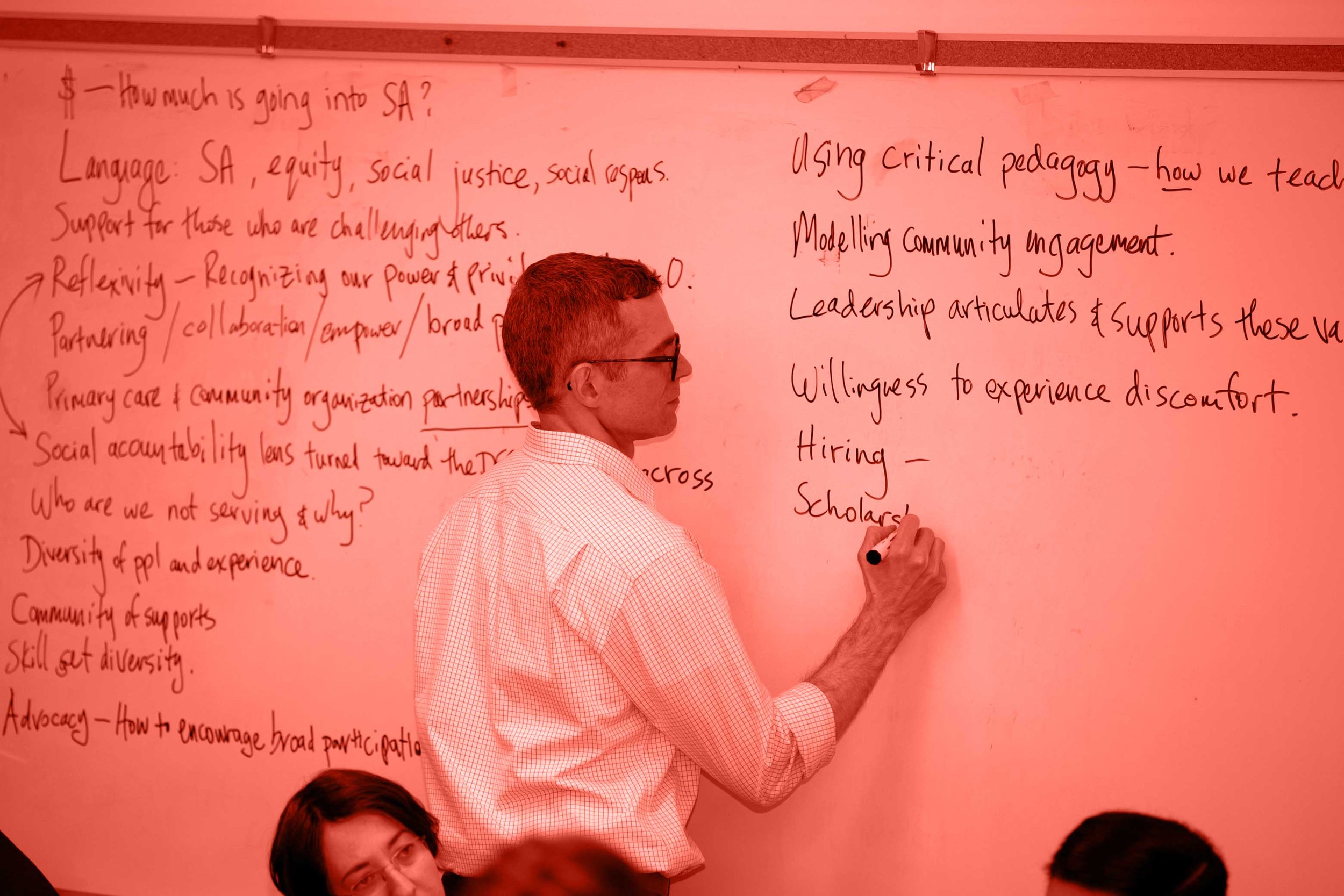
Having synthesized these inputs, we landed on several themes that we explored through 12 workshops, open to all members of the department, each focused on a specific topic. We discussed the “image and brand” of family medicine and the department, what it means to be socially accountable, and how we can meaningfully include wellness, arts and humanities in the department’s culture and work.
Through this active engagement, we reached approximately 500 people representing faculty, staff, learners, patients, partners, and more. We cannot guarantee that no voices were missed, but we believe this plan is a distilled expression of shared concerns and collective aspirations.
Through all of our engagement, clear themes, priorities, values and ambitions emerged.
We heard a strong need to prioritize learner and faculty wellness and to create and maintain anti-racist and anti-oppressive spaces for colleagues, learners and patients.
This entails a focus on inclusive and equitable care in our clinical and scholarly work, while also being brave about our own internal dynamics in the department. There is a need to create structures and processes that reduce imbalanced power dynamics, address inequity and build a more diverse and inclusive DFCM.
We heard about the need to grow our ability to practice community-level population health and focus on social determinants of health, making good on the “C” in DFCM and asking, “to whom are we accountable?”
We heard alignment and connection between challenges and potential solutions. For example, the need to support, revitalize, and increase our current and future workforce will naturally follow a healthier department and field. Therefore, we need to “build the small fires” — do the work internally to lead by example and build an environment that is constructive, safe and welcoming within DFCM.
Consistently, we heard the need to deepen our connections and opportunities for shared learning within our department, the healthcare community, and the communities that we serve. People expressed a deep desire for connection to one another. Simple and effective mechanisms for communication and collaboration were seen as critical for solution and information sharing, improved connectedness, and opportunities to continuously learn from each other.
As a department, we need to rethink our structures and roles to allow each of us to work at the top of our scope and to create space and resources for the areas of focus that have been identified as priorities. This includes not only our faculty members and learners, but also our staff, without whom DFCM would not function.
And we heard a desire to see us, together with partners, lead in re-establishing the value and role of family medicine and team-based care, propelling change in the healthcare system.
Despite the fatigue expressed by many, a hunger for courage in the face of that fatigue was made clear. We heard that we need to challenge the status quo, take bold risks, and be flexible, responsive & adaptable.
The aim of being a socially accountable department came through in many of our conversations. It is clear that this ambition resonates and it is also clear that what it means to be socially accountable varies. This plan sets out to ensure our department is socially accountable in a multitude of ways.
We want to be accountable to the public at large by building and supporting a workforce that allows for every person in need of a primary care provider to have one. We also want to ensure that this workforce is equipped to handle the ongoing challenges of COVID-19, the repercussions from this pandemic, and the pre-existing and ongoing challenges of changing demography, rising medical and social complexity, and health inequities.
We want to be accountable to First Nations, Métis and Inuit communities for supporting, resourcing and protecting the self-determination of Indigenous health leaders and communities and improving access and primary care attachment for these groups.
We want to be accountable to the most underserved and historically excluded communities by partnering with community organizations, listening to the needs of communities, prioritizing health equity in our education and research, and building care environments and approaches that are culturally responsive and adaptive.
We want to be accountable to our changing learner and faculty communities by creating environments that are safe, welcoming, and supportive in order to build and maintain a more diverse workforce that can respond to community needs.
We want to be accountable to the planet and to future generations by engaging in research, education and care that focuses on sustainability.
We want to be accountable to our learners by ensuring that what they are taught is reflective of the real and changing needs of patients, the healthcare ecosystem and structures they will navigate, and their own interests and concerns. This accountability includes continuing to support our graduates in the first five years of practice with ongoing training, mentorship, and connection so that they can be best equipped to provide the care their communities need.
We want to be accountable to every member of our department by foregrounding resources and tools for wellbeing, valuing non-traditional areas of impact such as community responsiveness and mentorship, and revisiting our roles and structures to help every member of the department have the time and capacity to work at their top of scope. We also want to work towards a more equitable distribution of resources amongst our sites so that we address health inequities. Furthermore, we want to improve the inclusivity of our department by equally valuing the roles of all members of healthcare teams.
We want to be accountable to the global community, bringing our expertise to meaningful and mutual international relationships in research, scholarship, policy and clinical care that build capacity to improve health outcomes around the world.
“Collectively we are better than each individual doing all of the things, all of the time.”
We want to be accountable to all those delivering primary care by offering expanded capacity building, continuing professional development, and inclusion in communities of practice.
And we want to be accountable to our health system partners by collaborating on health system reform initiatives, communications, and advocacy.
It’s a tall order, one that requires a newschool way of thinking, prioritizing and approaching our work.